Information On Diagnosing Crohn’s Disease

Crohn’s disease is a chronic intestinal disease located on the intestinal walls and other parts of the digestive tract. Its symptoms include diarrhea, abdominal pain and fever.
Inflammatory bowel diseases
Inflammatory bowel diseases (IBD) , or inflammatory bowel disease is the chronic inflammation of the intestinal wall, the origin of which is unknown. The inflammation is recurrent. The two biggest diseases are Crohn’s disease and ulcerative colitis ulcerosa.
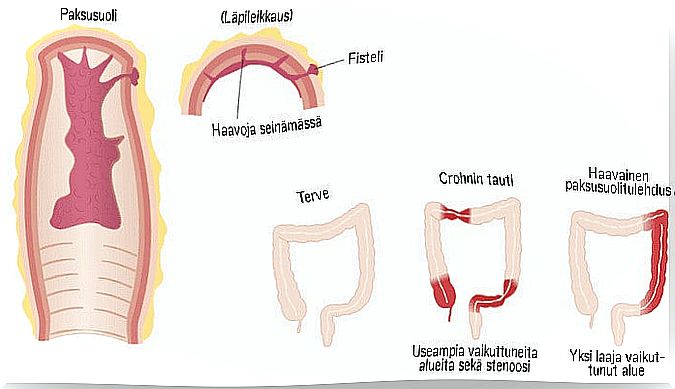
In inflammation of the ulcerative colon, the inflammation is located on the mucous surface of the intestinal wall. Crohn’s disease, on the other hand, affects the entire intestinal wall throughout its thickness and all parts of the intestine. It often acts in parts and in an asymmetrical way.
The origin of the disease is not known for sure. The most widely accepted theory of its origin is that the onset of the disease is influenced by many factors. In other words, the diagnosis of Crohn’s disease is the result of genetic, environmental, microbiological, and immunological factors.
Predictive symptoms of Crohn’s disease:
- diarrhea, often bloody
- stomach ache
- abdominal enlargement
- weight loss
- fatigue
- fever
The following complications of Crohn’s disease:
- abscesses
- fistula
- intestinal obstruction
- stenosis
- disease adjacent to the anus
- enlarged rectum
Individuals diagnosed with Crohn’s disease have been found to be susceptible to developing colon cancer. However, the results of the study are uncertain as the origin of the disease is unknown.
Extraintestinal manifestations
Intestinal manifestations in relation to disease activity:
- narrowing of the arteries
- nodule rose
- inflammation of the surface of the sclera of the eye, or episcleritis
- ulcerative stomatitis
- fatty liver
Intestinal manifestations independent of disease activity:
- skin ulcer disease
- psoriasis
- ankylosing spondylitis
- inflammation of the choroid of the eye
- Inflammation of the SI joint
Diagnosis of Crohn’s disease
The diagnosis of Crohn’s disease relies on clinical and histological examinations, laboratory tests, and endoscopic and radiological tests. There is no single specific test by which the disease could be diagnosed.
First, celiac disease and intestinal inflammation should be ruled out, as both cause inflammation of the intestinal walls.
Lack of effective research can lead to delays in the diagnosis of Crohn’s disease.
Look-out
The primary means of diagnosis is endoscopy. Endoscopy can be used to detect the prevalence and severity of the disease. It identifies the presence of the tumor (s) and evaluates the response and treatment.
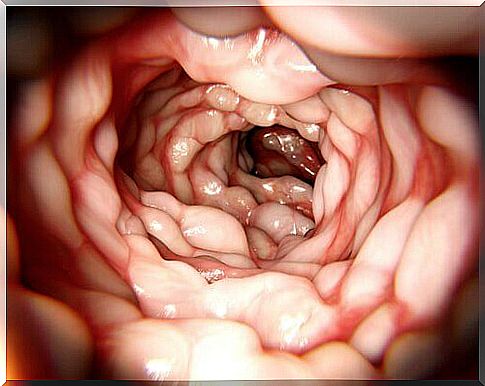
Prior to the diagnosis of Crohn’s disease, the situation is best assessed by colonic endoscopy.
Description
Different descriptions of different parts of the body are taken from the patient:
- ultrasound examination
- computer layer imaging or CT imaging
- magnetic resonance imaging
These help detect swelling, wounds, ankylosing spondylitis, rashes and ectopic disorders.
Histology
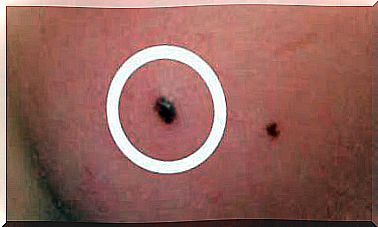
Taking a biopsy is an important part of diagnosing Crohn’s disease. These are characteristic of Crohn’s disease:
- granulomas
- lymphocytes or lymphocytes
- deformities of the intestinal walls
Laboratory tests
Your doctor will order a calprotectin test to check your stool protein levels. Based on this, it can be determined whether there is inflammation in the intestine. The result depends on whether this protein is found in the feces.
Crohn’s disease classifications
The Montreal classification system is used to classify patients, in which patients are classified according to the age at which the disease began, the location of the disease, and the behavior of the disease.
Age
- A1: under 16 years of age
- A2: 16-40 years old
- A3: over 40 years of age
Location
- L1: small intestine
- L2: colon
- L3: small and large intestine
- L4: limited upper gastrointestinal disease
Behavior
- inflammatory
- cramping
- fistulating, i.e. a hole becomes in the intestinal wall and a connection to another area of the intestine