Is Fibromyalgia Related To Intestinal Bacterial Growth?

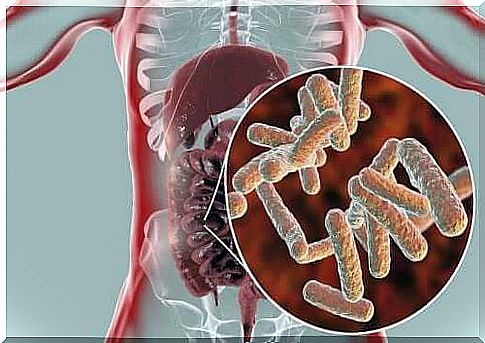
The intestinal bacterial growth is extremely fascinating and has been part of the most interesting studies in recent years. It is a collection of germs living in the gut that includes different types of bacteria, viruses and even fungi.
Intestinal bacterial growth has many irreplaceable purposes in the body. As many already know, these bacteria are essential for proper digestion. But that is not their only function in the body.
The composition of the bacterial culture can be associated with many different diseases, such as obesity. In this article, we report how chronic pain-causing fibromyalgia is associated with intestinal bacterial growth.
What is fibromyalgia?
Fibromyalgia is a complex disease that affects about 3 percent of the population. It is much more common in women than men. It is a chronic disease characterized by general pain in the muscles and bones.
There is no apparent cause for the pain. It is also usually associated with fatigue, insomnia, and mood swings. The reason seems to be a change in the way the brain processes pain stimuli, making the pain they cause feel more intense.
Doctors have found in many patients situations that trigger the typical symptoms of fibromyalgia. For example, they have found that it can be triggered by stress and infections. However, they had never noticed the connection of intestinal bacterial growth until quite recently.
How is fibromyalgia related to intestinal bacterial growth?
As we have already mentioned, the intestinal bacterial growth consists of all microbes living in the digestive system. They are bacteria, fungi and viruses that have a close relationship with the body.
Over the past few years, researchers have demonstrated how intestinal bacterial growth interacts with the body. Thus, the composition of the bacterial culture has an effect on many health-related factors. Every human being has a fundamentally different composition of bacterial growth.
A study by McGill University focused on monitoring intestinal bacterial growth in people with fibromyalgia. The study used samples from 156 women, 77 of whom suffered from fibromyalgia.
The study examined bacterial varieties living in the intestinal bacterial flora of each patient. The purpose was also to find out which bacteria were more and less in the body.
What was done in the study to monitor the intestinal bacterial growth in people with fibromyalgia?
In studying the intestinal bacterial growth of all of these people, the researchers found many differences in intestinal microbes in people with fibromyalgia. It was first found that the symptoms of the disease were associated with a change in the number of bacteria.
They also found that the severity of symptoms could be related to intestinal bacterial growth. Thus, for example, the number of certain bacteria was higher in people suffering from severe pain and fatigue.
The problem with this study was that it is still unclear whether changes in the intestinal microbial growth cause fibromyalgia or whether they are merely characteristics of this disease. In fact, the study focused more on the symptoms of pain. Researchers have yet to determine whether the same changes in intestinal bacterial growth occur with other diseases that cause chronic pain. That way, they will be able to see if they are really related to each other.

What does the connection between fibromyalgia and intestinal bacterial growth mean?
If intestinal bacterial growth is associated with fibromyalgia, it opens up a large number of new possibilities. For example, researchers could develop treatments and new diagnostic methods to help people better manage the disease. In fact, a change in the bacterial growth of the gut is currently used to treat certain diseases. Fibromyalgia is also a disease that can really make a person incapacitated, so this potential connection brings more hope for the future of patients with that disease.